No life without liver: how can we create systems that more closely resemble the human liver?
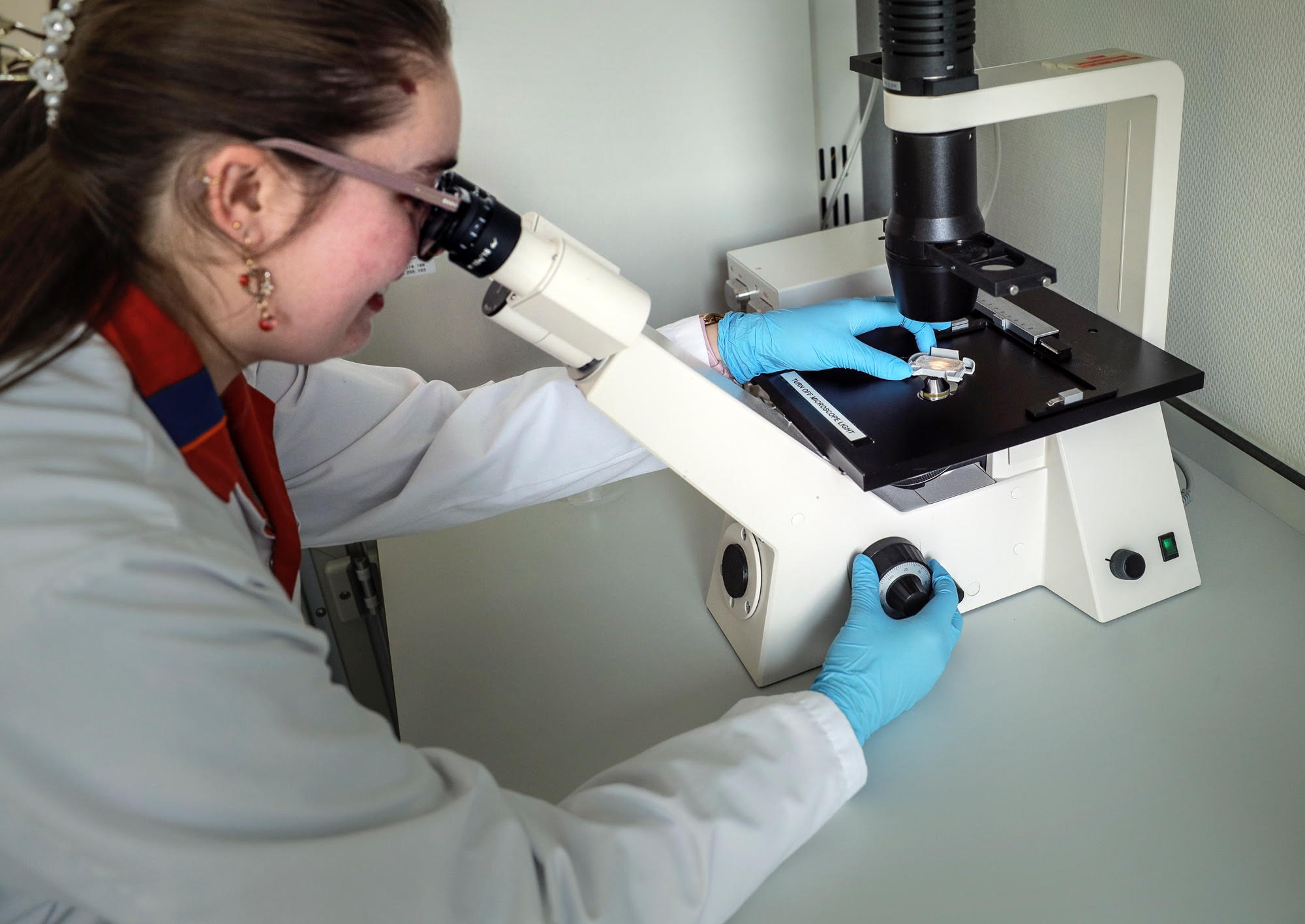
PhD student Victoria Palasantzas works both for the Department of Paediatrics and the Department of Genetics. This is where she is studying the effects of nutrients, such as antioxidants and fatty acids, on fatty liver disease. To do so, she is using a sophisticated liver-on-a-chip model: a hot topic in medical research.
Text: Victoria Palasantzas / Photos: Henk Veenstra
When I was a Master’s student I dreamt of combining my two main scientific interests: the use of diet in diseases and the development of model systems that do not require animals. I was given the opportunity to put my ideas in writing, defend my proposal in front of a committee, and won a research grant to implement this proposal, with thanks to my supervisors, Prof. Dr. Jingyuan Fu, Prof. Dr. Hans Jonker and Prof. Dr. Sebo Withoff. Since I work in two different departments, my days are very diverse, as far as work and colleagues are concerned. One day I culture liver cells, also called hepatocytes, to study fatty liver disease, while I try to create hepatocytes from stem cells the next day.

The role of the liver
My PhD programme revolves around the liver: our body’s multitasker. The liver is responsible for the production of bile, a substance that is essential for the digestion of food in our intestine. It also produces various coagulation factors, which are proteins that are necessary to stop bleedings. Furthermore, the liver plays a crucial role in detoxifying various substances in our body, including drugs and other toxic substances. Interestingly, every person has a different response because of their genetics, which leads to different activities of the enzymes that are responsible for detoxification. Moreover, the liver also plays an important role in the metabolism of sugars, fats, and proteins and, thereby, the body’s energy homeostasis. Because the liver has so many functions, it is not difficult to imagine that when something goes wrong in this organ, it will have a huge impact on your health. That is why it is very important that we study this fascinating organ and its role in health and the development of diseases.
Mimicking fatty liver disease
As part of my PhD programme, I am focusing mainly on fatty liver disease, also knows as MASLD (metabolic dysfunction-associated steatotic liver disease) in the medical world, and the ensuing inflammation. This pathology is often linked to unhealthy lifestyle factors, such as a chronically increased fat and sugar intake and physical inactivity. Let’s go back to the basics of metabolism to explain what a fatty liver is. After a meal, nutrients, including fats, are absorbed into our intestines and then into the bloodstream. The bloodstream delivers these nutrients to the various organs that need them. In addition, our body is also producing fats that end up in our blood. When there is an excess of these fats, they enter and accumulate in the liver. From a clinical perspective, a liver with a fat content of more than 5-10% of the total liver volume is considered a fatty liver.

Inflammatory response
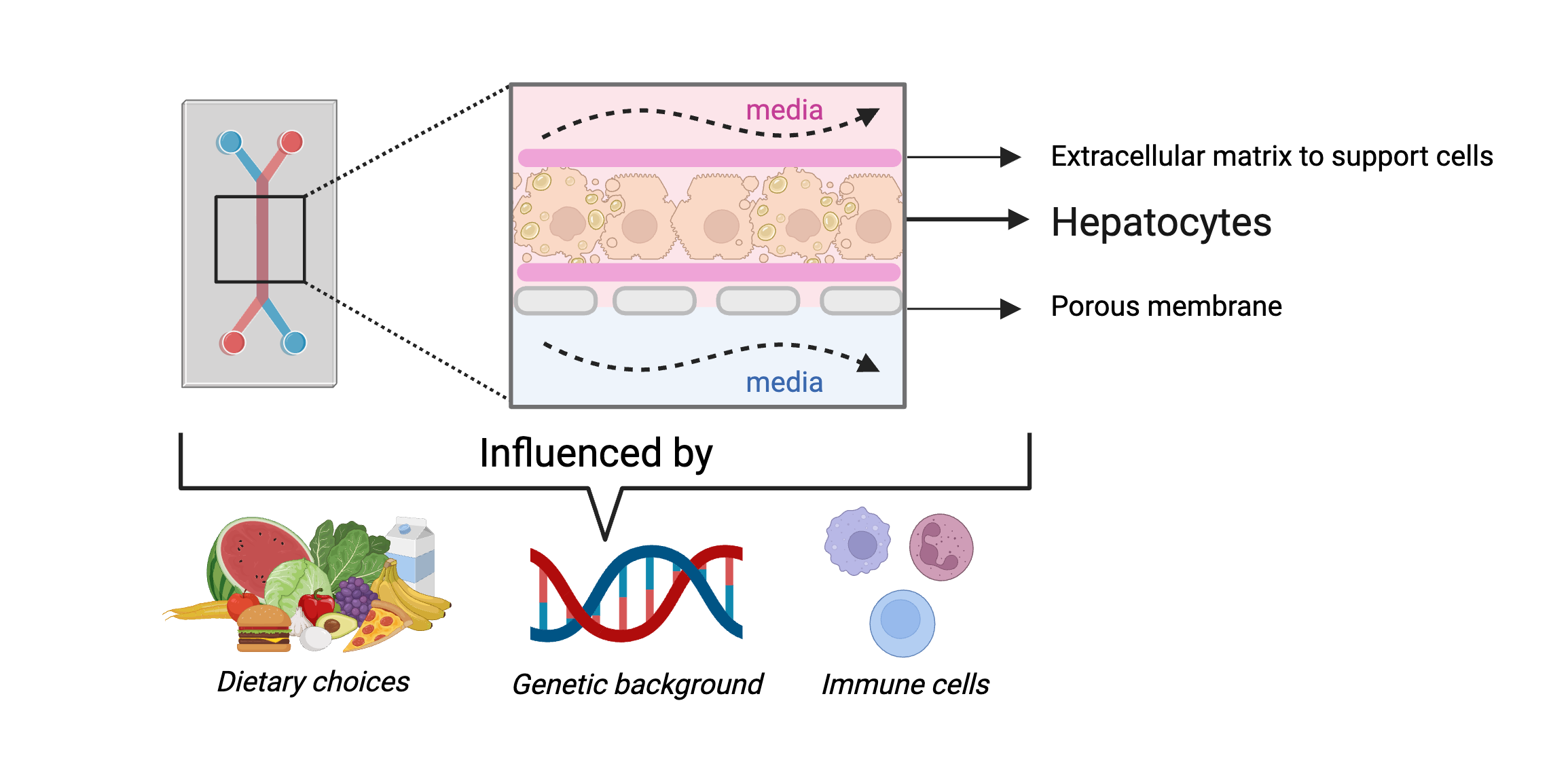
By developing a model system, I want to find out how the hepatocytes deal with this excess fat and whether these cells are still able to carry out their ‘normal’ tasks, such as releasing fats, and how they are prevented from carrying out these tasks. A fatty liver will also lead to complications in the long term, including inflammation in the liver. The hepatocytes become stressed and may even die, which will lead to the release of signals that something is wrong. Immune cells, which protect our body against infections and diseases, are then attracted to the liver and activated. In particular macrophages, immune cells that surround and destroy an infection, play a role in this. To better study the interaction between hepatocytes and macrophages, I am trying to introduce both cells into the same system so that we can study what happens during this inflammatory response and which genes or mechanisms are involved.

The liver-on-a-chip model
Of course, you would use a human liver in an ideal situation. However, that is not as easy as it seems because of the location of the liver in the body and the invasive procedure. That is why I am using a state-of-the-art technology: the liver-on-a-chip model, which resembles the human liver a little better, in terms of complexity, than traditional cell culture in petri dishes. A liver-on-a-chip model involves adding human cells, in this case hepatocytes, to a chip. These may be hepatocytes from healthy donors or from patients with an underlying pathology. These liver cells are supplied with a continuous flow of nutrients that, like the blood in the body, ensures that oxygen is delivered to the cells and that waste products are removed (see below). This creates an environment in which the cells can stay alive outside the body for a longer period of time. In addition to hepatocytes, it is possible to add other cells, such as immune cells, to study the interaction between cell types. A partially permeable membrane is positioned between these cell types, allowing the cells on both sides to communicate by means of signalling molecules. In part due to this system, the situation in the human body can be adequately simulated. This means that we can create a much more realistic situation without using laboratory animals.
Progress
So, in the group of Prof. Dr. Jingyuan Fu, I am working on the development of the liver-on-a-chip closely with Isabel Tamargo, Gwen Weijer and Dr. Joanne Hoogerland, and in a collaboration with the Netherlands organ-on-a-chip initiative (NOCI) and the Human Organ and Disease Model Technologies (hDMT). For this work, we use stem cells from healthy people, human induced pluripotent stem cells (iPSCs) to be precise. These stem cells have not yet developed into mature cells, which means that we are developing them from an unspecialized cell into a hepatocyte-like specialized cell. This involves a long protocol of approximately 40 days in which we let these stem cells progress through various stages of development using certain factors until they can be called hepatocyte-like cells. A significant challenge is making sure that they functionally resemble mature hepatocytes, like the hepatocytes in our livers. A potential problem when culturing cells that were originally stem cells is that these cells have more ‘fetal’ characteristics and do not always show all the characteristics of the desired cell type. Do you remember those detoxification genes that vary from person to person, the ones we mentioned earlier? They are poorly expressed in many hepatocyte cell models, such as the genes for the specific cytochrome P450 family (e.g. CYP3A4). That is why we are trying to improve the expression and activity of these genes in our liver-on-a-chip model.
Food as medicine?
Based on my interest in diet and diseases, my ultimate goal is to study the role of nutrients on the accumulation of fat in the liver. Specifically, I will study the effects of a number of substances in our diet that have known medicinal effects, also referred to as nutraceuticals, in a fatty liver disease model. These include antioxidants, which protect healthy cells and tissues, and short-chain fatty acids, which act as signalling molecules and as an energy source for your intestines. Many animal studies describe positive effects of these substances, although we have not been able to find much tangible evidence of that in humans. Therefore, in the follow-up of my research, I will use these nutraceuticals but also pharmaceutical drugs that are currently being developed for MASLD (such as obeticholic acid), in the liver-on-a-chip and see whether these affect the fat accumulation and inflammation in the liver. In short, I hope that my research will lead to the further development of systems that more closely resemble human tissues, using stem cells, the liver-on-a-chip model.
More news
-
17 November 2025
Artificial intelligence in healthcare
-
04 November 2025
AI Factory in Groningen advances digital sovereignty
-
03 November 2025
Menopause in perspective: How the media influences our perception
